Drinking Early in Pregnancy: A Comprehensive Guide
Introduction
Alcohol consumption during pregnancy has been a topic of concern for decades, with research consistently demonstrating the potential for adverse effects on fetal development. Understanding the risks associated with drinking early in pregnancy is crucial for expectant mothers and healthcare providers alike. This article provides a comprehensive overview of the potential consequences of alcohol exposure during the first trimester, examining the evidence, discussing the mechanisms of harm, and outlining recommendations for prevention and management.
First Trimester Alcohol Exposure: A Critical Period
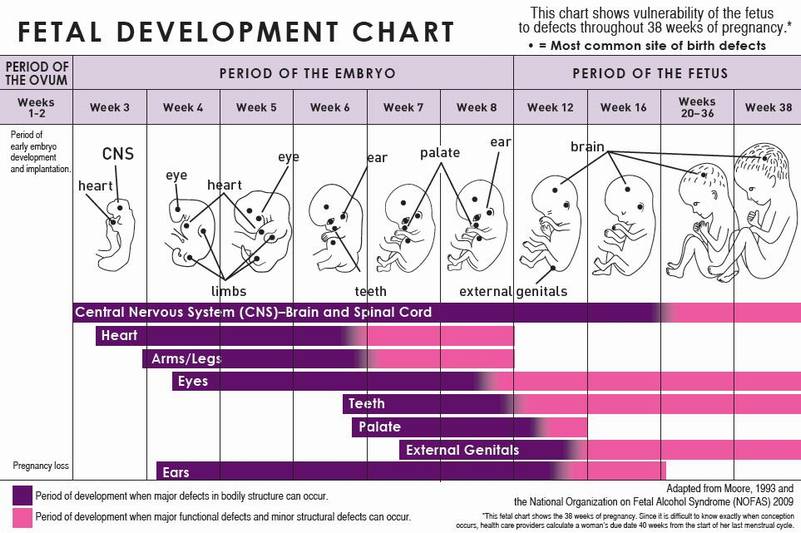
The first trimester of pregnancy, spanning from conception to week 12, is a period of rapid fetal development. During this time, the embryo and fetus undergo significant growth and differentiation, establishing the foundation for all future organ systems. Alcohol exposure during this critical window can disrupt these processes, leading to a range of developmental abnormalities.
Mechanisms of Harm
Alcohol readily crosses the placenta, exposing the developing fetus to its effects. Alcohol can interfere with cellular proliferation, differentiation, and migration, disrupting normal fetal growth and development. It can also alter gene expression, leading to long-term developmental consequences.
Potential Consequences
The potential consequences of drinking early in pregnancy are wide-ranging and can include:
- Fetal Alcohol Syndrome (FAS): FAS is the most severe form of alcohol-related birth defects, characterized by a distinctive facial appearance, growth retardation, and intellectual disabilities.
- Alcohol-Related Neurodevelopmental Disorders (ARND): ARNDs encompass a spectrum of neurocognitive impairments, including learning disabilities, attention deficits, and behavioral problems.
- Growth Restriction: Alcohol exposure can lead to intrauterine growth restriction, resulting in low birth weight and reduced fetal size.
- Cardiac Defects: Alcohol consumption during pregnancy has been associated with an increased risk of congenital heart defects, such as atrial septal defects and ventricular septal defects.
- Facial Dysmorphology: Alcohol exposure can cause distinctive facial features, including a flattened nasal bridge, short philtrum, and thin upper lip.
Evidence-Based Recommendations
Given the potential risks associated with drinking early in pregnancy, healthcare providers strongly recommend that women abstain from alcohol consumption throughout the entire pregnancy. This recommendation is supported by a wealth of scientific evidence and is consistent with the guidelines of major medical organizations, including the American College of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control and Prevention (CDC).
Prevention and Management
Preventing alcohol exposure during early pregnancy is paramount. Healthcare providers should routinely screen women for alcohol use and provide counseling and support to those who are drinking. Public health campaigns and educational initiatives can also play a role in raising awareness about the risks of alcohol consumption during pregnancy.
For women who have consumed alcohol early in pregnancy, it is essential to seek medical evaluation and counseling. While there is no known safe level of alcohol consumption during pregnancy, reducing or eliminating alcohol intake can mitigate the potential risks.
Conclusion
Drinking early in pregnancy poses significant risks to fetal development, with the potential for a range of adverse consequences, including FAS, ARNDs, growth restriction, cardiac defects, and facial dysmorphology. Healthcare providers strongly recommend that women abstain from alcohol consumption throughout the entire pregnancy. Prevention and management strategies, including screening, counseling, and public health initiatives, are crucial for protecting the health and well-being of both the mother and the developing fetus.